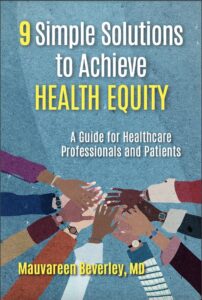
Dr Mauvareen Beverly discusses her book “Nine Simple Solutions to Achieve Health Equity.” Diving into the struggles of, African American seniors, and patients with, sickle cell disease. Dr. Beverly highlights, systemic biases, in healthcare and shares actionable strategies for ensuring equitable treatment. She emphasizes the importance of human value, cultural sensitivity, and patient engagement in transforming health outcomes.
Download the podcast here:
Key Takeaways:
Elderly black patients often face dismissive attitudes from healthcare providers, significantly impacting their health outcomes.
Cultural competence and sensitivity are critical in addressing health disparities within the black community, especially concerning chronic diseases like sickle cell.
Non-compliance labels in medical records perpetuate negative outcomes, necessitating a shift towards asking “why” and understanding patient perspectives.
Understanding Health Equity and the Dismissive Attitude Towards Elderly Black Patients
Elderly black patients have experienced a lifetime of societal and systemic biases, which continue to affect their healthcare interactions. Dr. Beverly notes that elderly black individuals often feel undervalued by their healthcare providers. “Doctors tend to be dismissive,” says Dr. Beverly, explaining that this stems from a long history of racial prejudice and unconscious bias in the healthcare system.
This dismissiveness has severe implications. African American seniors, have the worst health outcomes across all disease categories. Dr. Beverly’s work emphasizes that recognizing and countering this dismissal is crucial. For instance, the issue is not solely about access to healthcare but involves valuing the patient’s human dignity.
“If you don’t value me, my health is going to go south,” she asserts.
Healthcare providers must adopt a non-judgmental, empathetic approach and listen to patients’ stories. Dr. Beverly recounts a poignant interaction with a patient who said, “My parents were a step away from slavery, and my grandparents were slaves.” These stories highlight the historical trauma contributing to mistrust and poor health outcomes. A team effort focused on cultural sensitivity and patient engagement reduced readmission rates dramatically from 30% to 18.7%, showcasing the power of empathy and understanding in healthcare.
Sponsored Link
Ignite the Passion in your Relationship with a Pheromone Perfume
The Crucial Role of Cultural Competence and Sensitivity
Cultural Competence Defined
Cultural competence and sensitivity are not just buzzwords but essential components of effective healthcare, particularly for black Americans. Dr. Beverly emphasizes the need for healthcare providers to understand the cultural context of their patients. It’s not just about language barriers; it’s about a profound understanding of the patient’s background and how it influences their health and behavior.
For example, sickle cell disease, predominantly affects the African American community in the United States. Patients with this condition often face stigmatization and are dismissed as drug seekers. “The notion that because I have, Sickle cell disease, you will refer to me as a drug seeker is unconscionable,” Dr. Beverly states. She points out that these patients are often undertreated, leading to repeated visits to the emergency room.
Dr. Beverly’s solution was to start a sickle cell support group. Engaging directly with patients revealed deep-seated issues. “You doctors don’t teach me about sickle cell; sickle cell teaches me,” one patient said. These insights underscore the importance of incorporating cultural competence into medical training and practice. Empathy, respect, and an understanding of the patient’s lived experience can transform healthcare outcomes and health equity.

Addressing Non-Compliance Labels for Better Health Equity
The Impact of Language in Medical Records
One of the most pressing issues Dr. Beverly highlights is the use of the term “non-compliant” in medical records. This term often disproportionately affects black patients and has significant negative health outcomes. “If you in the hospital or with your doctor, and they didn’t ask you if you followed directions or took the medication, wait a couple of seconds and ask, ‘Do you want to know why I didn’t take the medication?’,” advises Dr. Beverly.
The word “non-compliant” creates a stigma that can lead to patients being neglected or receiving substandard care. Dr. Beverly stresses the importance of asking “why.” Understanding the reasons behind a patient not following medical advice can lead to better care plans and improved health outcomes.
In her advocacy, Dr. Beverly educates both patients and healthcare providers about the detrimental effects of this language. She suggests that patients assertively request that the term “non-compliant” not be used in their medical records without understanding the context. This proactive approach could shift the dynamics in healthcare, making it more inclusive and effective.

Recapping the Essential Themes for Health Equity
The journey to achieving, health equity for black Americans, particularly the elderly and those with chronic conditions like sickle cell, involves several key strategies. Firstly, addressing the dismissiveness in healthcare by valuing patients and listening to their stories can dramatically improve health outcomes. As Dr. Beverly’s work demonstrates, empathy and patient engagement lead to tangible improvements, such as reduced readmission rates.
Secondly, cultural competence and sensitivity must be integrated into healthcare practices. Understanding the patient’s cultural background and the systemic issues they face can alter the course of treatment for the better. Dr. Beverly’s sickle cell support group initiative is a testament to the power of cultural competence in healthcare.
Finally, rethinking the language used in medical records, especially terms like “non-compliant,” is crucial. Asking “why” and understanding the patient’s perspective can lead to more effective and compassionate care. Dr. Beverly’s advice for patients to advocate for themselves and question stigmatizing labels is a powerful step towards health equity.
Conclusion
In summary, achieving, health equity for black Americans, requires a multifaceted approach that includes empathy, cultural competence, and a critical examination of systemic practices within healthcare. By focusing on these areas, we can move towards a more equitable health system where every patient is valued and heard.